Could a low thyroid be responsible for infertility? Here’s how these two medical problems are related – and what to do about it.
As many as 20 million Americans struggle with a thyroid problem of some kind, and these numbers continue to increase each year. More than 12 percent of the U.S. population will develop a thyroid condition at some point in their lives, and women are five to eight times more likely to have thyroid problems than men. As many as 60 percent of those who have thyroid disease don’t even know that their thyroid is having problems.
At the same time, more than 12 percent of women have difficulty getting or staying pregnant. Is there a correlation between thyroid issues and infertility?
How Often is the Thyroid Involved in Fertility Problems?
As much as four percent of women battling infertility also suffer from hypothyroidism, or low thyroid function, as part or all of their infertility issue. That’s approximately three to four million women in the United States alone.
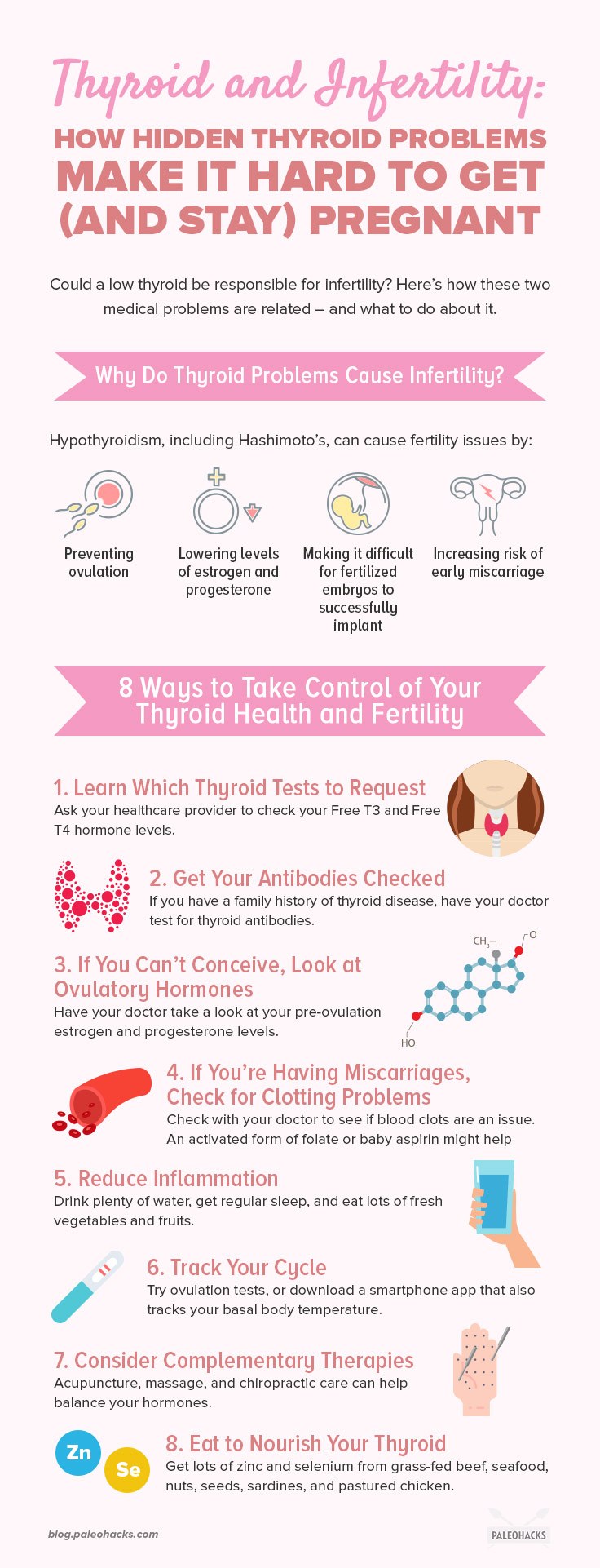
Hypothyroidism, including the autoimmune form of Hashimoto’s, can cause fertility issues by:
- Preventing ovulation
- Lowering reproductive hormone levels of estrogen and progesterone
- Making it difficult for fertilized embryos to successfully implant
- Increasing risk of early miscarriage
Without healthy thyroid hormones, pregnancy can’t be effectively sustained. In fact, thyroid dysfunction can have major impacts on women’s health in general, including menstrual cycle length and hormone imbalances.
Bottom line: The thyroid is essential for women’s health, including fertility. When levels are off, even without detectable symptoms, the effects can be significant.
Why Thyroid Problems Go Undetected
A common way to monitor thyroid health is to test something called TSH, short for thyroid-stimulating hormone. This hormone is actually produced by the pituitary gland which is a small endocrine organ about the size of a pea that is located near the base of the brain.
The pituitary gland is supposed to tell the thyroid when to make more hormone, and the reasoning is that if the pituitary is working extra hard to get this message through, then thyroid hormone levels must be low. The trouble with this approach is that for this to be completely accurate, hormonal communication needs to be healthy – and it often isn’t if one or more endocrine organs aren’t doing their job.
Sometimes thyroid hormone output can be low, but the pituitary isn’t communicating the need for more, so TSH levels return as “normal.” Additionally, the range of normal for TSH is so broad that many patients can have symptoms of low thyroid even when they fall in the normal range.
Low levels of thyroid hormone can result in skewed reproductive health, slowed ovulation, and a higher risk for miscarriage.
Holistic medicine, instead, tests for free-circulating thyroid hormones in the blood to assess how the thyroid is really functioning. Ideally, the body keeps these levels stable on their own, though in cases of hypothyroidism or Hashimoto’s, these hormones can be suppressed.
Low levels of thyroid hormone can result in skewed reproductive health, slowed ovulation, and a higher risk for miscarriage.
Pregnant women with known thyroid issues should seek extra thyroid monitoring right away since pregnancy can change the amount of hormone needed. Ensuring that the thyroid is properly managed can help to reduce the risk of miscarriage.
Bottom line: Checking for TSH is an outdated way to monitor thyroid health. Find a practitioner well-versed in thyroid-associated infertility to ensure the best detection and care.
8 Ways to Take Control of Your Thyroid Health and Fertility
Every woman is unique in how infertility and thyroid health affect one another. Sometimes thyroid problems cause infertility, while other times, they are only one part of a woman’s infertility challenges. Empower yourself with these top eight things you need to know about thyroid health and fertility.
1. Learn About Thyroid Tests (and Go Beyond TSH)
If your doctor is only testing for TSH, request getting checked for free-circulating thyroid hormones by asking specifically for Free T3 and Free T4. It’s important that you get the “free” versions, as these are the most accurate way to assess actual thyroid hormone available to your cells.
Most doctors will require that these tests be done after fasting overnight and before you take any thyroid medications. Your first test will essentially be a baseline. If you’re out of the normal range, it will give a goal to work toward with medication. If you’re in the normal range but at the low end, and still experiencing problems, you may still require a boost of medication to get you to the optimal part of the range for you. After a few tests, you’ll have a good gauge of where you feel best.
2. Get Those Antibodies Checked
You should also get tested for thyroid antibodies if you have a family history of thyroid disease or any kind of autoimmunity. If you’ve been diagnosed as hypothyroid but you can’t seem to get your thyroid under control, ruling out autoimmune causes can help to pinpoint the next steps.
There are two kinds of thyroid antibodies:
- TPO (thyroid peroxidase antibody) – Signals that the immune system is attacking the thyroid, either in overactive or underactive autoimmune disorders.
- Thyroglobulin antibody – Attacks the stored form of thyroid hormones or T4.
People with autoimmune thyroid problems may test positive for one or both antibodies, and the results may be low or high. If there are any antibodies present, it’s time to start looking at gut health as the cause of autoimmunity.
3. If You Can’t Conceive, Look at Ovulatory Hormones
If your thyroid is off-kilter and you’re having trouble getting those two pink lines on a pregnancy test, it’s time to take a closer look at your pre-ovulation estrogen and the other hormones that control it: FSH (short for follicle-stimulating hormone) and LH (luteinizing hormone).
Together, these hormones control the development of the egg and uterine lining, and the timing of ovulation. If any of these are off, then the chances of conceiving are quite slim.
After ovulation, it’s also important to have the right hormones, like progesterone, to support the fertilized embryo. Thyroid hormones have a hand in regulating these reproductive hormone levels, so take a closer look at all of these throughout your cycle to get a better idea of where the problem lies.
4. If You’re Having Miscarriages, Check for Clotting Problems
There are many reasons why a woman might have a miscarriage, but clotting problems are a common cause. The embryo needs to implant in a uterine lining rich with nourishing blood, and if there are problems with blood flow, it can spell disaster for an early pregnancy.
Clotting problems can range from genetic to autoimmune. In some genetic cases, taking an activated form of folate can help to downplay clotting troubles. In other situations, baby aspirin or low-dose blood thinners can help.
5. Reduce Inflammation
Inflammatory problems can cause chaos in the body, including the reproductive system. Not only can inflammation mess with hormonal balance and communication, but it can cause other fertility problems, like an inflamed uterine lining, an acidic vaginal canal (which rejects sperm), and even autoimmune attacks against the uterus or an embryo.
To reduce inflammation, be sure to drink enough water, get regular sleep, and eat plenty of vegetables and fruits. Avoid dietary sensitivities of all kinds.
6. Track Your Cycle
Even if you have a cycle that works like clockwork, tracking it can provide valuable information for your healthcare provider.
Download a smartphone app that gives you the option to chart your temperature. Taking your body temperature every single morning can be a helpful way to identify thyroid problems as well as pinpoint issues with pre- or post-ovulation hormones.
If you want to take it one step further, you can also use ovulation tests, which help to track your ovulation time, sometimes down to the hour.
7. Consider Complementary Therapies
While complementary therapies like acupuncture, massage, and chiropractic care can’t necessarily cure infertility or thyroid issues, they can help to rein in symptoms or to bring some level of balance.
Acupuncture has been shown to improve thyroid functioning, and can also help to improve fertility when it comes to uterine blood flow, reproductive hormone balance, and even implantation success. Certain forms of therapeutic massage have also been shown to improve fertility and pregnancy rates.
8. Eat to Nourish Your Thyroid
A diet rich in vegetables, fruits, healthy fats, and proteins is essential for hormone balance, especially the thyroid. In particular, zinc and selenium are two key nutrients that are commonly deficient in people with low thyroid function.
Zinc is found in foods like red meat, seafood, nuts, and seeds, while selenium is present in Brazil nuts, sardines, grass-fed beef (particularly the liver) and pastured chicken. In some cases, thyroid patients with fertility issues can benefit from extra supplemental zinc and selenium while they’re trying to balance their levels.
Avoiding foods that interfere with thyroid function is just as essential as eating the right ones. Processed foods, dairy, gluten, and soy are the worst offenders for thyroid hormones and fertility. Because it naturally avoids all of these, Paleo is an excellent fertility diet and can help to provide nutritional balance for anyone who is battling with underactive or autoimmune thyroid problems.
Bottom Line
While there isn’t a single approach for addressing thyroid and fertility problems where you can get accurate testing and pursue a treatment plan that meets your individual needs, you will find greater success at both managing your thyroid condition and improving your conception and pregnancy success rates.